At SynApps we are continuously looking for ways to improve our solutions to the benefit of our customers. One such area of focus is centred around standards-based interoperability by allowing collaborating hospitals to establish a Vendor Neutral Imaging Network (VNIN). But what is a VNIN?
A Vendor Neutral Imaging Network (VNIN) is a healthcare-related concept that refers to an interoperable and standardized system for the storage, exchange, and retrieval of medical images. It is designed to overcome the limitations of traditional Picture Archiving and Communication Systems (PACS), which often have proprietary formats and communication protocols, making it challenging for healthcare facilities to share medical images seamlessly.
The primary objective of a VNIN is to create a platform where medical images, such as X-rays, CT scans, MRIs, ultrasounds, and other diagnostic images, can be shared across a region in a standardised manner. This enables healthcare providers, including hospitals, clinics, and imaging centres, to efficiently access patient images and data across different facilities and systems, regardless of the vendor or manufacturer of the equipment used to generate the images.
Key features and characteristics of a Vendor Neutral Imaging Network include:
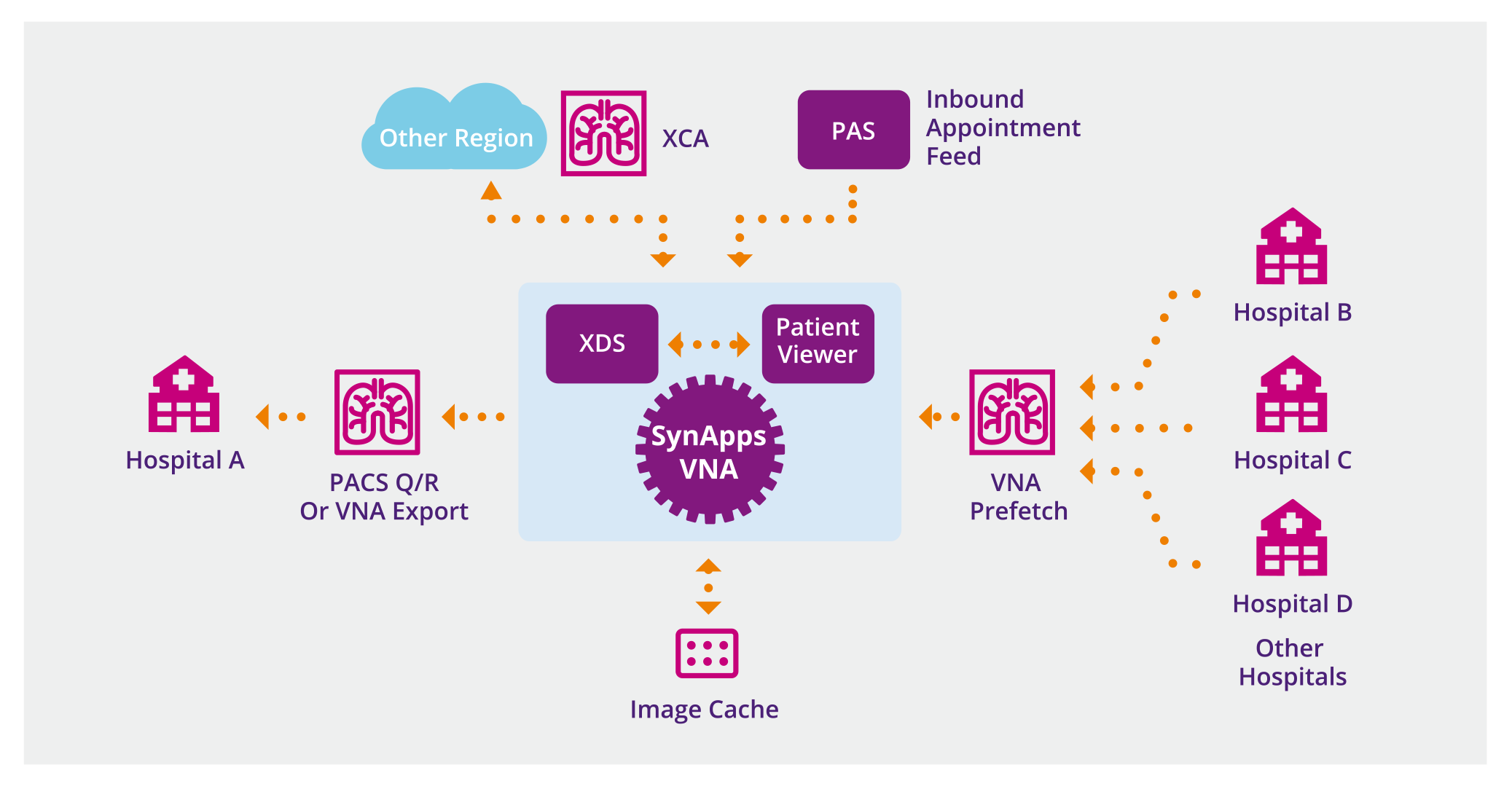
- Standardization: VNINs adhere to industry standards, such as DICOM (Digital Imaging and Communications in Medicine), FHIR (Fast Healthcare Interoperability Resources), XDS (Cross-Enterprise Document Sharing) and XCA (Cross-Community Access), which ensure that medical images are stored and communicated in a uniform format. These standards allow different systems to communicate, understand and interpret the images consistently.
- Dynamic Interoperability: VNINs are designed to support the dynamic on-demand sharing and retrieval of Patient Images and Documents across a region of collaborating hospitals without mandating the creation of a single central archive. VNINs can be integrated with other regional or national XDS registries to support wider information sharing.
- Centralized Image Repository: Since a VNIN supports the dynamic sharing of information, a central repository is not mandatory. However, VNINs may also provide a centralised storage repository for medical images to improve scalability, accessibility or resilience depending on the need.
- Scalability: VNINs are scalable to accommodate the growing volume of medical images generated daily. This is essential as medical facilities continue to adopt digital imaging technologies and generate increasingly larger datasets.
- Security: Given the sensitivity of medical images and patient data, VNINs implement robust security measures to protect patient privacy and comply with relevant regulations, such as General Data Protection Regulation (GDPR) and the Health Insurance Portability and Accountability Act (HIPAA) in the United States.
- Vendor Independence: As the name suggests, a VNIN is vendor-neutral, meaning it is not tied to any specific medical equipment manufacturer. This independence allows healthcare facilities to choose imaging devices from different vendors while maintaining seamless data exchange.
- Access Control and Authorization: VNINs implement access controls and authorization mechanisms to ensure that only authorized healthcare professionals can access and view patient images.
- Data Integrity: VNINs prioritize data integrity, ensuring that medical images remain accurate and unaltered during storage and transmission.
By adopting a Vendor Neutral Imaging Network, healthcare organizations can improve clinical workflow efficiency, enhance collaboration among specialists, and ultimately deliver better patient care by ensuring that critical medical images are readily accessible and shareable across the healthcare ecosystem.
The SynApps VNIN solution offers these critical features alongside an advanced zero footprint diagnostic viewer which can further extend access to not only other clinicians within the hospital but also those users within the community or primary care who may not have historically had direct access to such critical patient data.